Highlighting Structural Drivers of Health Disparities to Bolster Support for Addressing Inequality: Evidence from Survey Experiments with Purposive Diverse Samples
People of color drive engagement: Black, Hispanic, and Asian respondents expressed stronger concern, policy support, and advocacy intent than White respondents, with Black participants showing the highest levels of engagement.
Structural messaging works: Explanations of systemic drivers of poor health (e.g., housing segregation) increased recognition of root causes and policy support without eliciting backlash from White respondents.
Actionable path forward: Communicators should contextualize disparity data and prioritize disproportionately affected communities’ perspectives to mobilize change.
Why We Did This Study
While COVID-19 exposed profound racial health disparities, quantitative studies aiming to understand public attitudes about disparities have historically prioritized White Americans’ perspectives, underrepresenting the most affected groups—Asian, Black, and Hispanic communities (Niederdeppe et al., 2023). This exclusion has critical policy implications: prior work found White respondents shown disparity data without structural context exhibited reduced support for mitigation policies (e.g., lower mask-wearing intent). But how do the communities experiencing these inequities respond to this information? And how might context explaining the systemic factors – like housing segregation and employment conditions that compounded COVID-19 risk — affect public understanding and response?
Our studies address this evidence gap by:
- Purposively sampling the four largest racial/ethnic groups (Asian, Black, Hispanic, and non-Hispanic White)
- Testing whether structural messaging (e.g., linking disparities to housing segregation, occupational risks) mitigates potential backlash and amplifies engagement among marginalized groups.
Disparity Only:
“Furthermore, COVID-19 infection is 400% more likely to lead to the hospitalization of Black compared to White U.S. residents…”
Structural Explanations:
“These differences in COVID-19 infections and deaths are due to longstanding patterns of discrimination. Historically, many of the laws and policies enacted by legislators have had the effect of limiting where Asian, Black, Indigenous, and Latino/a people live. … As a result, they are more likely to live in densely populated neighborhoods… conditions that make it much easier for COVID-19 to spread…”
How We Did This Study
We conducted two survey experiments (2023- 2024) with an analytic sample of 2,896 participants in Study 1 and 6,627 in Study 2, intentionally sampling the four largest U.S. racial/ethnic groups to address historical underrepresentation in health disparities opinion research. Using a randomized design, participants viewed either: (1) disparity-only statistics highlighting unequal COVID-19 outcomes, or (2) structural explanations linking these disparities to systemic factors like housing discrimination or occupational risks.
Study 2 replicated and extended these methods during a later pandemic phase, using identical measures while streamlining some attribution questions to focus on structural causes and advocacy intentions. Both studies accounted for demographic variables, with analysis comparing effects across and within racial/ethnic subgroups —particularly marginalized communities’ responses relative to White participants. Study 2’s pre-registered design and materials are publicly available via Open Science Framework.
What We Found
Our research revealed both consistent patterns and important variations in how communities responded to COVID-19 disparity messaging across two national studies. While structural messaging increased recognition of systemic causes and policy support for all racial groups in Study 1, these effects were weaker in Study 2—though Black and Asian participants maintained the strongest belief in structural causes throughout both studies. Most strikingly, Black respondents consistently demonstrated the highest levels of engagement across all measures, showing the greatest support for mitigation policies, willingness to take individual and collective action, and attribution of disparities to government systems. We also observed unexpected shifts between studies: where structural messaging initially increased COVID-19 fear specifically among Black participants in Study 1, this effect expanded to all racial groups in Study 2. Notably, significant response variations emerged within racial groups—particularly among Hispanic and Asian subgroups—underscoring the need for more nuanced research on the implications of racial categorizations.
Crucially, three core findings remained stable: (1) marginalized communities showed the deepest engagement with health equity issues, (2) systemic explanations did not trigger backlash, and (3) persistent racial gaps in policy support and advocacy willingness endured despite changing pandemic contexts.
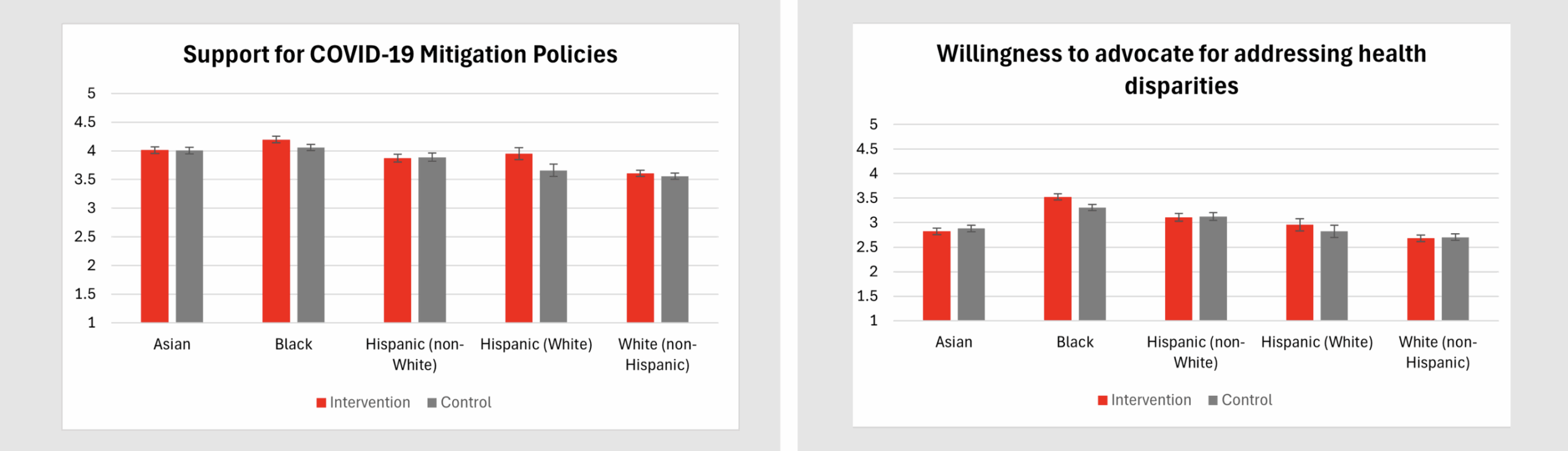
*Intervention messaging provided structural explanations for racial disparities, while Control messaging presented disparity rates without additional causal context.
What These Findings Mean
This research reveals that equitable health communication demands three critical shifts: centering underrepresented voices, embedding structural narratives, and aligning policies with communities most affected—and most ready to drive change.
Our studies demonstrate that Black, Hispanic, and Asian Americans consistently showed greater concern, policy support, and mobilization intent than White respondents, but with no negative responses among White respondents. These findings align with our team’s recent study on messaging about child tax credit (CTC) expansion, which similarly found that discussing the targeted benefits of the policy on reducing poverty among children of color increased policy support across racial groups without backlash.
The consistency of marginalized groups’ responses across both studies highlights the need to examine how intersectional identities (e.g., class, immigration status) further shape engagement. Additionally, both studies assessed immediate messaging effects; longer-term impacts of repeated exposure remain untested. Nevertheless, the lesson is clear: when research intentionally amplifies marginalized voices—whether in health equity or economic policy—it uncovers pathways to change that benefit all communities. By combining structural narratives with policy efficacy evidence (e.g., CTC expansion’s poverty reduction or COVID-19 mitigation successes), practitioners can build messaging that mobilizes without polarizing.
Key Recommendations
- Center marginalized communities: Prioritize Black, Hispanic, and Asian voices—groups that showed the highest advocacy willingness in both our COVID-19 and CTC studies.
- Pair data with structural explanations: Use narratives that link inequities to root causes (e.g., “Overcrowded housing from redlining increased COVID-19 risk”) to strengthen policy support.
- Test targeted universalist framing: As our CTC study demonstrated, messages can highlight racial disparities within universal benefits without alienating White audiences.
Acknowledgement
This work was funded by the Robert Wood Johnson Foundation (Grant #79754). The views expressed here do not necessarily reflect the views of the Robert Wood Johnson Foundation.
We thank Monica Cornejo for her feedback on this project and are grateful for the support of the entire Collaborative on Media & Messaging for Health and Social Policy.
This research brief is based on the following study:
Lewis, N. Jr., Porticella, N., Liu, J., Taylor, T., Michener, J., Barry, C. L., Nagler, R. H., Gollust, S. E., Moore, S. T., Fowler, E. F., & Niederdeppe, J. (July 2025). Beyond fear of backlash: Effects of messages about structural drivers of COVID-19 disparities among large samples of Asian, Black, Hispanic, and White Americans. Social Science & Medicine. Advance online publication, https://www.sciencedirect.com/science/article/pii/S0277953625004265
Citation
Suggested Citation:
Lewis, N. Jr., Porticella, N., Liu, J., Taylor, T., Michener, J., Barry, C. L., Nagler, R. H., Gollust, S. E., Moore, S. T., Fowler, E. F., & Niederdeppe, J. (May 2025). Highlighting structural drivers of health disparities to bolster support for addressing inequality: Evidence from survey experiments with purposive diverse samples [Research brief]. COMMHSP. https://commhsp.org/highlighting-structural-drivers-of-health-disparities-to-bolster-support-for-addressing-inequality/